The HIV Estimates 2023 Factsheets, shared by the National AIDS Control Organisation (NACO), a division of the Union health ministry, with all states in June this year, also showed that India had 25.44 lakh people living with HIV (PLHIVs) in 2023, up from 24.67 lakh in 2022. These figures do not dispute the historical success of India’s HIV-AIDS programme but, at the same time, do not look flattering at all.
Instead, alarm bells ring on a closer look — after a consistent decline for a decade (2010 to 2020), the annual new HIV infections and PLHIVs began to rise in 2020, and the trend has continued. India logged 1.2 lakh annual new HIV infections in 2010, which by 2020 had dropped to 57,550, but there were 62,970 new infections in 2021 and 66,000 in 2022, showcasing an increasing rate of infections.
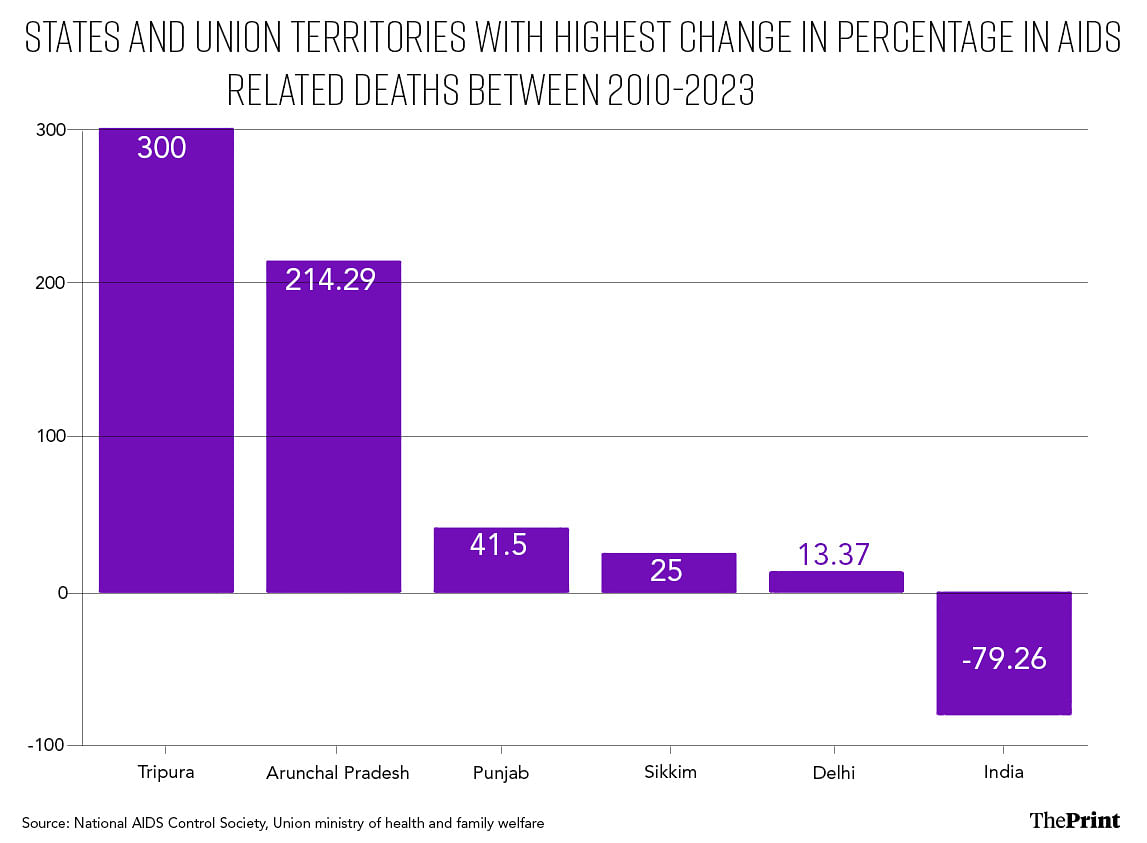
In 2023, Punjab, Bihar, Uttar Pradesh, Maharashtra and Andhra Pradesh registered the highest number of annual new HIV infections among all Indian states, in absolute numbers. However, since 2010, the rate of new HIV infections has declined in all the states except Punjab.
In contrast, in four states, Tripura, Arunachal Pradesh, Meghalaya, and Assam, apart from Union Territory Dadra and Nagar Haveli and Daman and Diu, the rate of new HIV infections has risen since 2010. In Tripura, the rise in annual new HIV infections was 524 percent in 2023 compared to 2010, the highest among all states. This figure was roughly 470 percent in Arunachal Pradesh, 124 percent in Meghalaya and 116 percent in Punjab.
However, in Mizoram, Nagaland, and Manipur — which still have the highest percentage of adult (15–49 years) HIV prevalence per 1,000 population in the country, mainly due to injectable drug abuse — the rate of new infections has declined.
The trend of rising annual new HIV infections in a select few states, mainly those witnessing increasing levels of injectable drug abuse such as Tripura, has experts worried.
“This is unacceptable,” said Dr Ishwar Gilada, president emeritus of the AIDS Society of India (ASI) and formerly associated with NACO’s technical guideline committee.
The worst part is that more than 70 percent of new HIV infections are among marginalised communities that already face an extreme degree of stigma and discrimination, Gilada said.
Dr R.R. Gangakhedkar, epidemiologist and former chief scientist (communicable diseases and epidemiology) at the Indian Council of Medical Research (ICMR), said India has come a long way in curbing AIDS, but there are challenges.
“The COVID-19 pandemic hit the National AIDS Control Programme (NACP) adversely, and the trend of rising new infections in some states is very worrying,” Gangakhedkar, who has also headed the ICMR-National AIDS Research Institute previously, told ThePrint.
ThePrint reached NACO director general V. Hekali Zhimomi, over phone calls and emails for a comment on the challenges India faces in curbing the epidemic. This report will be updated if and when a response is received.
This is the second story in ThePrint’s two-part series on the status of India’s National AIDS Control Programme and HIV infections in the country.
Also read: ‘Udta Tripura’ — HIV cases are soaring in hill state, with youth under 30 worst hit
All focus on treatment, prevention takes backseat

Twenty years ago the central government introduced free Antiretroviral Therapy (ART) for all PLHIVs. It was a crucial decision, which proved to be one of the key interventions in the fight against HIV, which is mainly transmitted through body fluids such as blood, semen and vaginal discharge and from infected mothers to unborn babies.
India’s generic drug manufacturers are considered the backbone of the global AIDS response. It is estimated that these Indian companies make over 92 percent of antiretroviral medicines that keep PLHIVs healthy worldwide.
As part of the free ART programme, the use of multidrug regimens, which substantially reduce the progression to AIDS, opportunistic infections, hospitalisations, and death, is typically offered to all PLHIVs, including asymptomatic individuals, regardless of their immune status.
Gilada pointed out that in 2021, NACO launched the NACP V programme, which will continue till 2026, to reduce new infections.
However, new infections have only increased over the last three years.
“NACP III, on the other hand, was launched in 2007 to halt and reverse the AIDS epidemic by the end of 2012 and later extended to 2014. The target was achieved to a great extent. But then, NACP lost grip on prevention and intervention activities after its major focus and budget allocations shifted to ART and viral load monitoring,’’ Gilada said.
The major HIV awareness and prevention campaigns witnessed during 2000-2010 are now missing. Gilada said that children born during that period, now in their teenage years or adulthood, missed the prevention campaigns and are now falling victim to HIV and other sexually transmitted infections.
According to experts, the key tools for preventing new infections, especially among high-risk groups, are pre-exposure prophylaxis or PReP and self-testing kits, apart from awareness campaigns. Both PReP and self-testing kits are not included in the NACP yet despite recommendations by the NACO technical resource group.
PrEP refers to the use of antiretroviral medication to reduce the risk of acquiring HIV, especially among individuals at high risk of HIV. Research suggests that if used correctly and consistently, it can reduce the risk of HIV by over 90 percent among those who are sexually active and by nearly 70 percent among those who inject drugs.
“The lack of these prevention measures fuelled new HIV infections all over India,” Gilada said.
NACO estimates that the HIV prevalence among high-risk groups in India continues to be much higher than the overall adult prevalence.
In comparison to the estimated national adult prevalence of 0.20 percent in 2022, the observed HIV prevalence among high-risk groups is 9-43 times. The HIV prevalence is 1.85 percent among female sex workers, 1.93 percent among inmates in central jails, 3.26 percent among men who have sex with men, and 3.78 percent among transgender persons, according to NACO data.
But the highest prevalence, 9.03 percent, is among injecting drug users.
“The states seeing a rise of IDUs do need aggressive preventive measures, especially among the high-risk groups,” said Dr Shrikala Acharya, public health specialist with the King Edward Memorial Hospital in Mumbai and earlier associated with the Maharashtra AIDS Control Society.
Also read: With AIIMS Delhi set to train surgeons in face transplant, a look at the procedure & risks involved
Short on target, checking vertical transmissions & TB deaths
In 2014, the United Nations set 95-95-95 treatment goals, which aim to diagnose 95 per cent of all HIV-positive cases, provide antiretroviral therapy (ART) for 95 percent of those diagnosed, and achieve viral suppression (so infection does not spread to sexual partners) for 95 percent of those treated.
But till March 2023, according to a NACO report, only 79 percent of PLHIVs knew their HIV status. Among the PLHIVs who knew their HIV status, 86 percent were on ART. Among those on ART, viral load suppression was achieved in 93 percent.
“Like most other countries with significant HIV high burden, we too are far short on the 95-95-95 target,” said Dr Glory Alexander, a Bengaluru-based HIV specialist and member of the International AIDS Society.
Another problem, according to specialists, is that a huge 11.75 percent of the infections are by vertical transmission — infected mothers passing on the virus to unborn babies.
“It suggests that the HIV programme is falling awfully short of achieving viral load suppression in pregnant women living with HIV,” said Gilada.
Another challenge has been HIV patients falling prey to highly infectious bacterial diseases such as tuberculosis (TB).
According to the latest WHO Global TB Report 2023, roughly 48,000 TB patients in the country also had HIV, and 11,000 of them died of TB.
“When TB is preventable and curable, even one TB death is a death too many. We can save lives if we ensure people with HIV are on effective ART and protected against TB,” Dr Dilip Mathai, the president of the AIDS Society of India, said during the ASI annual session in March this year. “If HIV patients get co-infected with TB, early and accurate diagnosis and linkage to TB care is lifesaving.”
(Edited by Madhurita Goswami)
Also read: ICMR back in race to offer world’s 1st vaccine for deadly shigella, to tie up with Indian manufacturer

