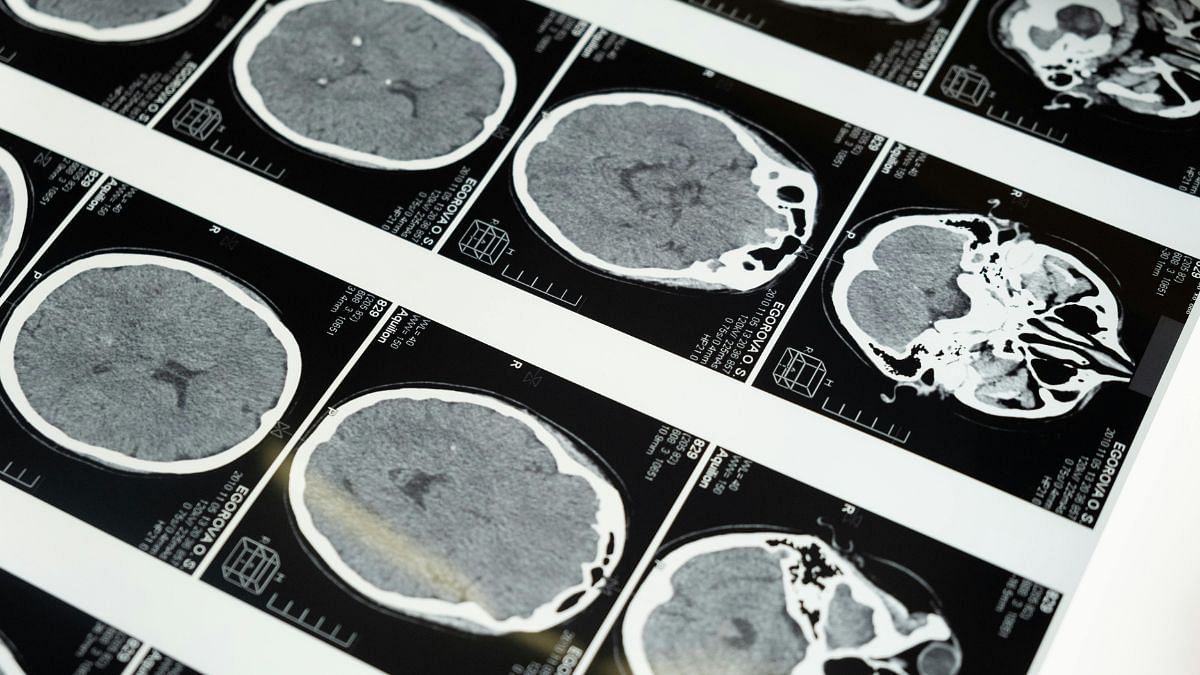
Bengaluru: Neuroscientists from the Tata Institute of Fundamental Research (TIFR)-Mumbai, in collaboration with international researchers, have identified the neuron type in the brain responsible for modulation of anxiety. The landmark study utilised synthetic psychedelic DOI (2,5-Dimethoxy-4-iodoamphetamine) directly injected into rats’ brains to identify the neural circuits involved in anxiety.
DOI is a psychedelic whose effects are comparable to LSD, but the drug does not have an established safety profile and is not used as a street drug. Such psychedelics have shown tremendous benefits in treating mental health disorders such as depression in recent times, and the process is accompanied often by the hallucinatory effects these drugs produce which causes individuals to see distortions of vision.
The team initially identified that among all the serotonin receptors in the body, including in various parts of the brain and even the gut, only those in the ventral hippocampal region—the part of the brain that regulates stress- and emotion-motivated behaviors—directly affected anxiety response in the mice, decreasing it in experiments. The neural circuit that was involved in reducing anxiety was also different from the circuit involved in hallucinatory effects, which in mice and rats manifests as a head twitch response.
Subsequently, within the ventral hippocampal region, the team then identified the population of neurons that fired while lowering anxiety.
In a significant achievement in neuroscience, they were then able to modulate anxiety by simply simulating these neurons, called PV-positive neurons, to fire entirely without the psychedelic.
“This is the first study that has delineated an entire circuit for a certain kind of neuropsychiatric disorder with psychedelics. In that context, it is a huge step forward in the field,” said lead author Praachi Tiwari, neuroscientist, who has just begun her postdoctoral fellowship at the Center for Psychedelics and Consciousness Research at Johns Hopkins, after her Neuroscience PhD at TIFR-Mumbai, which resulted in this paper.
The findings from the study are expected to lead to potential development of novel synthetic drugs in the same family as DOI, but without any psychedelic, hallucinatory effects.
The findings are among many groundbreaking studies conducted in recent times on the neurochemistry of mental health disorders like depression and anxiety, with psychedelics that are known to activate receptors across the brain and show promising results. The study was published in the journal Neuron Tuesday night (IST).
Also read: Chandrayaan-3’s Pragyan rover landed in previously unknown crater, one of the oldest on the Moon
Experiment & discoveries
Disorders like anxiety, depression, and OCD, have overlapping neural circuits responsible for them in the brain’s network. Therapeutics that target them are designed to, typically, latch on to serotonin receptors in the body and brain.
In recent years, there has been a resumption of initial research from the 1960s and 1970s in psychedelics and their effects on brain chemistry. Notably, psychedelics have shown tremendous promise in treating and reversing depression.
“There have been many studies on depression, but there is quite a paucity of research on anxiety and psychedelics,” explained Tiwari. “So, we set out to understand what happens, by working with the idea of serotonin signalling with psychedelics.”
The team at TIFR worked on albino rats, well documented and understood in scientific literature, in a set up called an elevated plus maze (EPM). The maze contains two elevated arms crossing each other like a plus sign. One arm contains tall walls while the other one is open and exposed to light and the elements, and the rodents can move between the arms in the middle of the plus sign.
Rats generally prefer to be within the walled arm, and when they venture out, often return quickly owing to baseline anxiety and fear. When anxiety was reduced, in the experiments, the rats would stay out in the light and wind for longer periods of time.
To understand which region of the brain DOI worked on in the rats, the study team mapped multiple regions of the brain in great detail before delivering the drug to that specific region alone. They identified receptors in the ventral hippocampal region of the brain. When these receptors were blocked and then the drug delivered, there was no anxiety-modulation effect.
They were also able to demonstrate that the hallucinatory effect and anxiety effect induced by the same drug worked on different parts of the brain.
Brain circuits for anxiety
To understand the way the drug worked in the rat’s body, project lead Vidita Vaidya, neuroscientist at TIFR and last author on the paper, draws an analogy to providing the drug to a city to observe what lights up. Say, if the drug were given to everyone in Mumbai, researchers could see which areas of the city respond to it.
“First we have to figure out which part of the city is actually responding and lighting up,” she said. “We initially figured out that, say, something lit up in the Marine Drive region. Now within here, there are many buildings, and we had to figure out which building is actually the one getting lit up. Finally, we identified that, say, it is the singular Air India building that is being lit up by this drug.”
In effect, the team found that DOI was causing a specific population of neurons in the ventral hippocampal region of the brain, called PV-positive interneurons, to fire rapidly and light up. This activation of these neurons was identified as the mechanism that tempers anxiety in these rats.
The team then decided to take it a step further. If the drug was going and turning on the lights in one specific building, they wanted to know what would happen if they simply turned on the light switches in there instead of delivering the drug. The researchers directly simulated these PV-positive neurons and caused them to fire without the use of the psychedelic drug, and discovered that it indeed did result in reduction of anxiety.
The findings show that other drugs that could cause these PV-positive interneurons to fire could potentially lead to therapeutics in anxiety, obtaining the anxiety-lowering effect of a psychedelic without even the use of it.
“This project highlights the complexity in what psychedelics do to the brain. The drug can get into many different brain regions and affect different cell types,” said Alex Kwan, neuroscientist at Cornell, formerly at Yale when he led the team who co-authored the study.
The study, which was conducted over a period of five years, saw teams from TIFR-Mumbai collaborating with Yale, Cornell, and Columbia Universities, as well as New York State Psychiatric Institute.
“The collaboration made too much sense to pass up, and we jumped at the opportunity. Her intuition was correct—we found, exactly as she predicted, that the fast-spiking cells were firing aberrantly after a dose of psychedelic, supporting Vidita’s behavioural results,” he said.
(Edited by Zinnia Ray Chaudhuri)
Also read: Elon Musk’s implant could help the blind see. All about Blindsight that got FDA ‘breakthrough device’ tag