Bengaluru: The deadly sickle cell disease (SCD), which causes blood cells to deform into a sickle shape, could potentially have two cures by the end of the year. A new gene therapy from the American biopharmaceutical company Vertex Pharmaceuticals would be the first to be able to cure sickle cell disease provided it is approved by the US federal drug regulator FDA by December.
The FDA is scheduled to review the therapy this week. A second therapy by another American company, the Massachusetts-based Bluebird Bio Inc., is also expected to be reviewed by the agency by the year’s end.
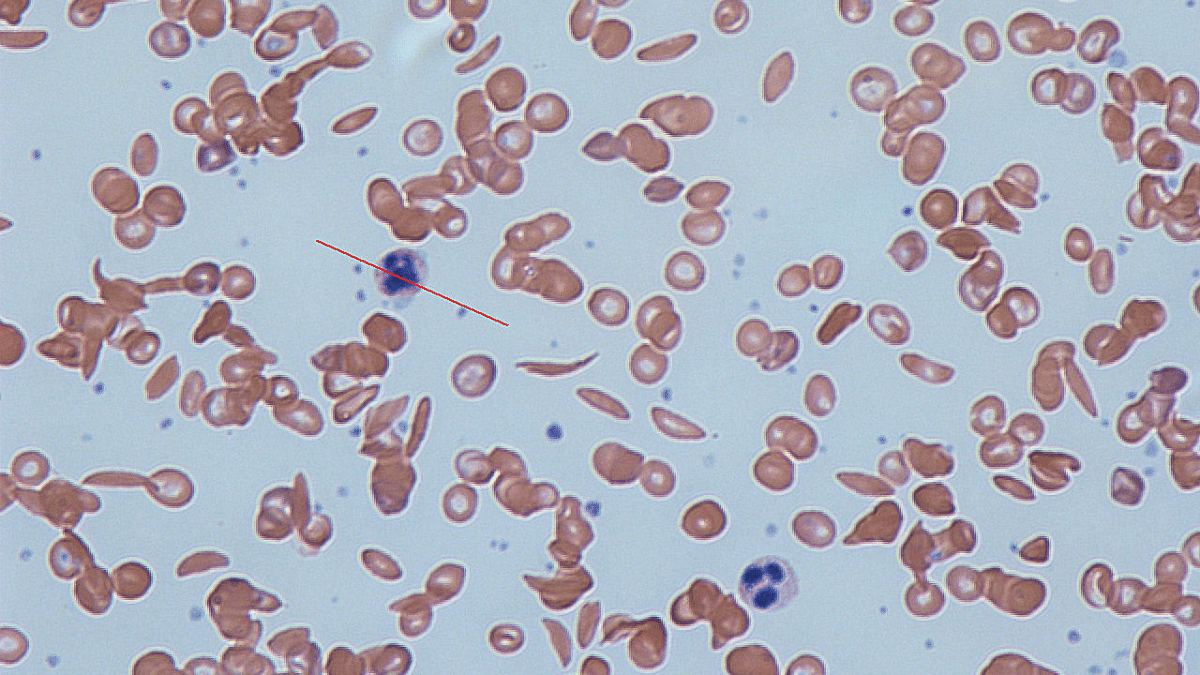
The genetically inherited SCD causes cells to die early, depleting red blood cells that carry oxygen, and causing a severe form of anemia leading to excruciating pain and serious damage to organs. It’s diagnosed through a blood test, and treatments include blood transfusion, IV fluid intake, folic acid, penicillin, and pain medication.
The more severe cases of the disease can also lead to severe infections, strokes, bone and kidney necrosis, hypertension, and cardiac issues.
The development could mean a breakthrough for the disease, which so far, has no definitive cure that could apply to everyone, although there are some treatments. The average life expectancy is about 40 years.
Also Read: All about India’s 1st ‘living drug’ that uses patient’s own genetically engineered cells to fight cancer
Two new gene therapies
The treatment expected to be approved first is called exa-cel (for exagamglogene autotemcel), and is made by Vertex Pharmaceuticals. It utilises the CRISPR gene-editing technique and reverses the mutation that causes the disease.
Short for “clustered regularly interspaced short palindromic repeats”, CRISPR is a technology that scientists use to selectively modify the DNA of living organisms.
For the process, pluripotent stem cells, which can develop into healthy red blood cells, are removed from a patient’s body and edited in the lab.
A stem cell is a cell with the unique ability to develop into specialised cell types in the body while a pluripotent stem cell can grow into any other cell of the body.
CRISPR allows researchers to remove the genetic mutation that leads to the production of deformed cells, thus resulting in the production of healthy red blood cells. These edited stem cells are transplanted back into patients after chemotherapy, leading to the subsequent production of healthy cells.
Since it is a permanent change to the DNA, it is a one-time treatment and no donor is required.
In its July 2023 report titled ‘Gene Therapies for Sickle Cell Disease’, the Institute for Clinical and Economic Review — a Boston-based healthcare nonprofit — cites Vertex as saying that 46 people had been enrolled in its trials. Of these, 30 patients had follow-ups for 18 months and there was no hospitalisation for pain or disease.
During the review process, the FDA will extend its research to find unintended consequences of genetic change before giving its approval.
On the other hand, Bluebird Bio Inc’s therapy — called ‘lovotibeglogene autotemce’ — does not utilise CRISPR. This is also a one-time gene therapy, where individuals with the disease will receive an additional functional gene that can produce anti-sickling adult hemoglobin.
According to the company’s press from June this year, results from its trials on 36 patients with an average follow-up of 32 months showed safety and efficacy.
Six of the 36 patients were followed up for more than six years — the longest of any gene therapy, according to the press release.
Both therapies are expected to be expensive, costing more than SCD treatments like bone marrow transplants and blood transfusion, which on average come to over $1.7 million.
What is sickle cell disease?
SCD disease occurs when a foetus inherits two abnormal copies of the beta globin or HBB gene, which is responsible for haemoglobin production. A person with a single copy of abnormal cells, inherited from one parent, does not carry the disease but does carry the genetic mutation that can be passed down.
The mutation evolved as a means to protect the body against malaria in Sub-Saharan Africa, where the disease is still most prominent.
It occurs mostly in tropical regions, including central and South Asia. People who can trace their ancestry to Sub-Saharan Africa are also at a higher risk of inheriting the disease.
So far, the only available cure for SCD is a bone marrow transplant, which helps produce newer and healthier red blood cells, although the lack of suitable bone marrow donors poses severe challenges.
(Edited by Uttara Ramaswamy)
Also Read: New hope for HIV cure: Dual gene editing ‘eliminates’ infection, targets protein that helps virus enter body