Gurugram: Haryana is facing a severe shortage of healthcare professionals, which has adversely affected the quality and accessibility of medical services, a report released this week by the Comptroller and Auditor General of India (CAG) revealed.
Based on a performance audit of public health infrastructure and management of health services in Haryana conducted from 2016 to 2021, the report says that data has been updated up to 2022-2023, wherever feasible.
The report covers various aspects of healthcare including financial management, human resources, service delivery and adequacy of healthcare infrastructure. “This assessment aims to align Haryana’s healthcare services with the goals set forth in the National Health Policy (NHP) 2017 and Sustainable Development Goal 3 (SDG-3), which focuses on ensuring healthy lives and promoting well-being for all ages,” it reads.
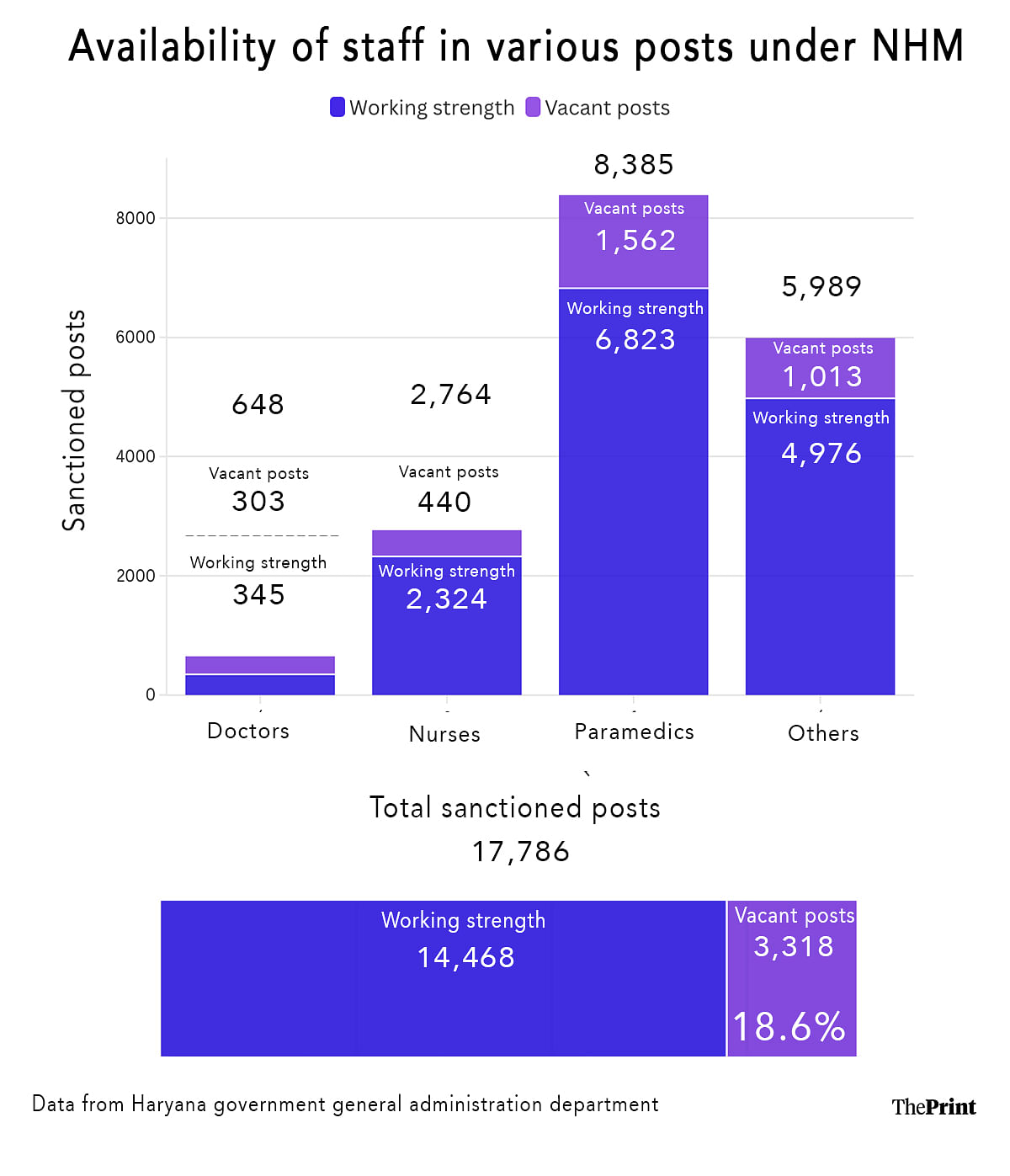
Tabled in the Haryana assembly during its winter session on 13 November, the report shows that nearly 41.8 percent of the total sanctioned posts across various healthcare directorates have remained vacant, with the biggest shortages observed in the food and drug administration (56 percent), AYUSH (55 percent) and Director General Health Services (DGHS) (40 percent).
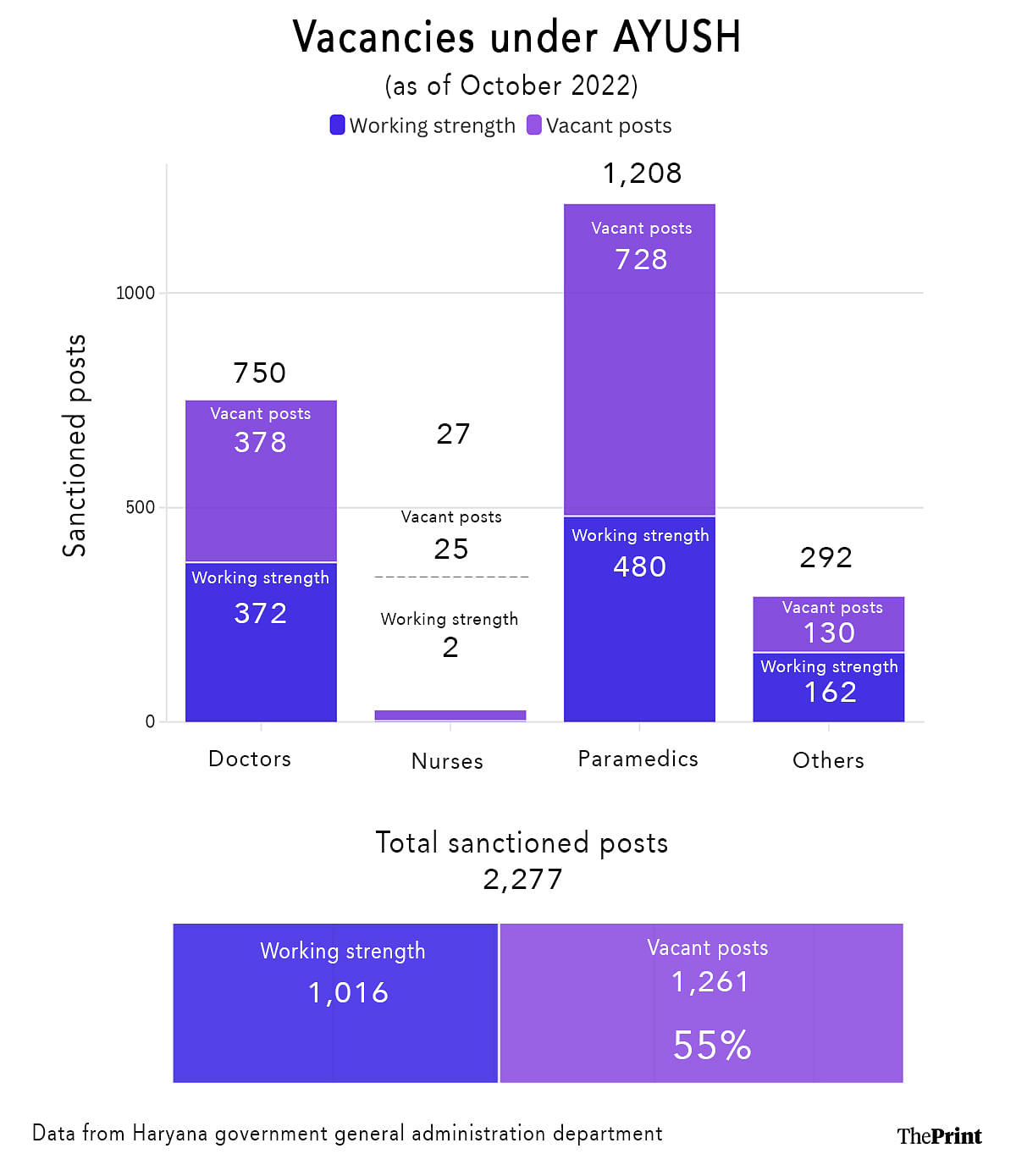
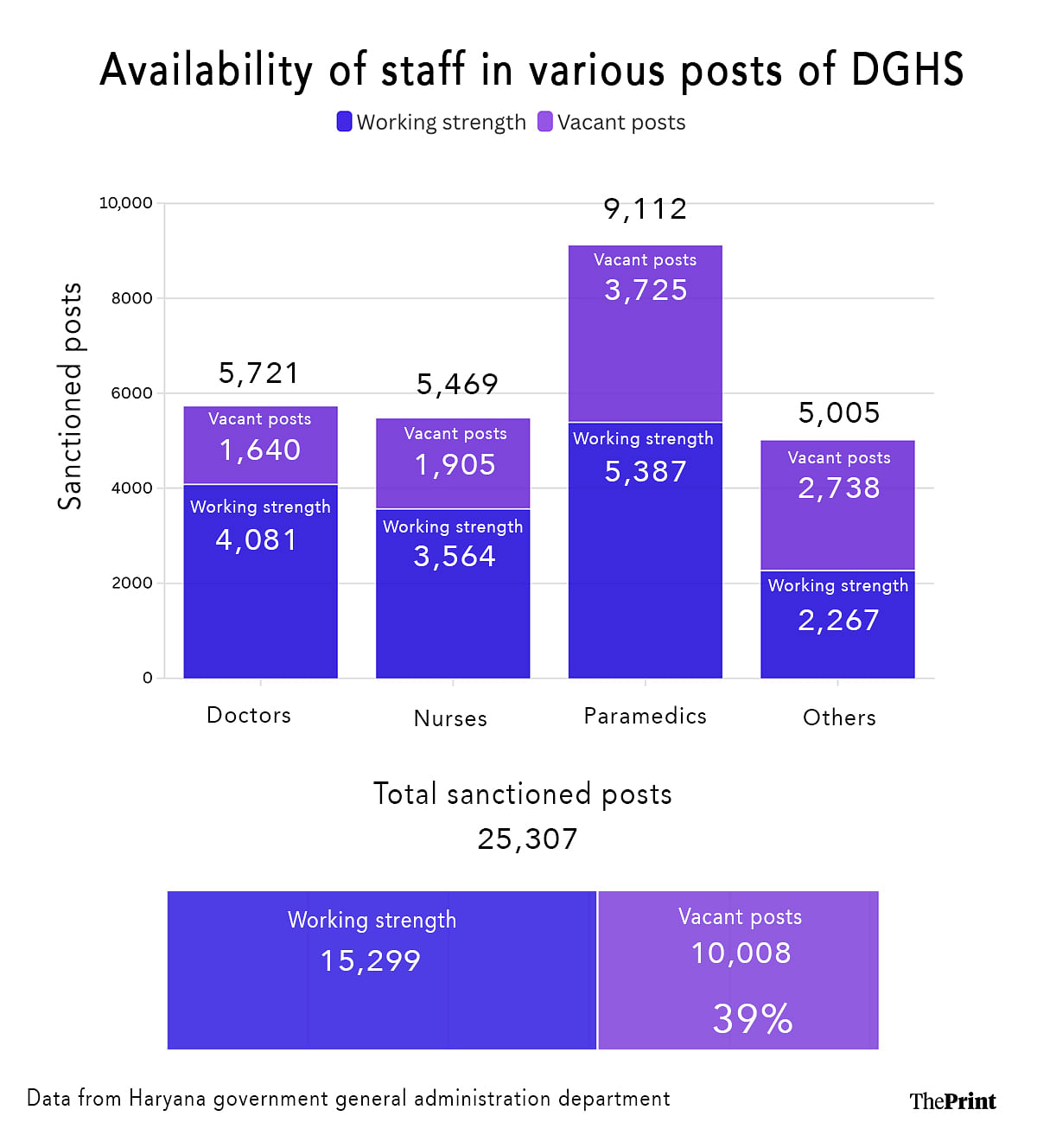
Within DGHS, positions for doctors, nurses, paramedics and other healthcare professionals showed alarming vacancy rates. The percentages of positions for doctors, nurses and paramedics which remained unfilled were 28.7, 34.8 and 40.9, respectively.
Key positions such as those of radiographers, ultrasound technicians and ECG (electrocardiogram) technicians were severely understaffed.
At a district level, disparities were stark. For instance, Rohtak had a vacancy rate of just 14.9 percent and Yamunanagar 57.5 percent.
This uneven distribution means that districts with higher vacancy rates face greater difficulties in offering essential services, exacerbating regional health disparities.
The report further notes that “the sanctioned posts were also not as per population as population to doctor ratio ranges from one doctor sanctioned for 2,339 people in Panchkula district to one doctor sanctioned for 9,999 people in Faridabad district”.
In Kaithal, which has a population of 10.74 lakh people according to the 2011 census, there are 105 doctors including specialists, against a sanctioned strength of 207, a shortage of almost 50 percent.
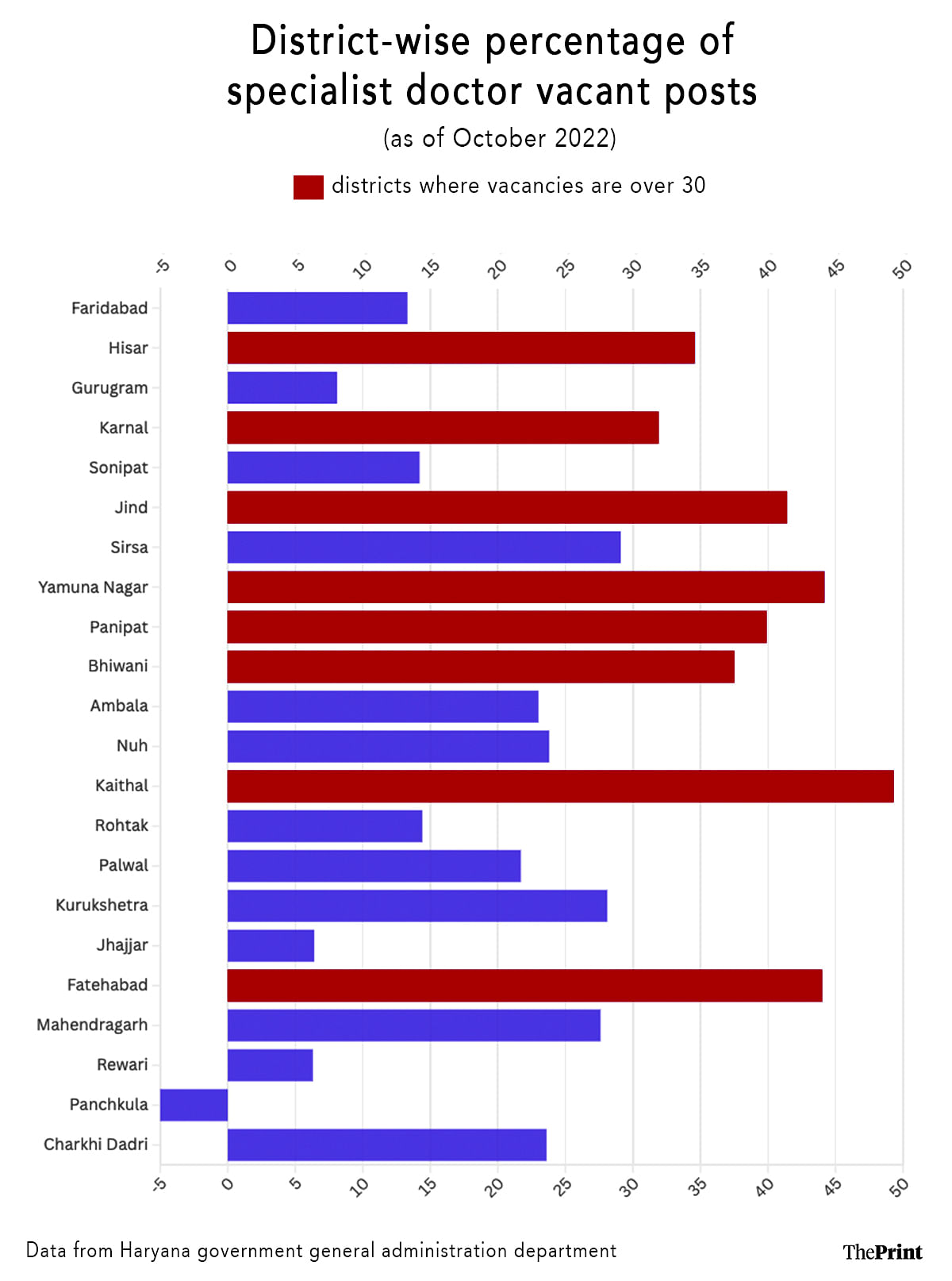
Moreover, the state’s shortage of specialists such as anaesthetists, paediatricians and gynaecologists particularly affects rural healthcare facilities, which are often entirely dependent on these roles for specialised care.
The lack of a specialist cadre in district hospitals (DHs) and community health centres (CHCs) has rendered these institutions unable to meet Indian Public Health Standards (IPHS) in many locations. Across DGHS facilities, the demand for support staff remains unmet, with 54.7 percent of these positions left unfilled.
The CAG report adds that while some gaps are covered by contractual hires such as those employed through the National Health Mission (NHM), this temporary workforce solution remains insufficient to address the growing healthcare needs in Haryana.
It underscores the need for the state government to accelerate recruitment and ensure an equitable distribution of healthcare workers to strengthen the public health system and improve service delivery.
Besides this, the Directorate of Medical Education and Research (DMER)—which runs five medical colleges across Karnal, Faridabad, Sonipat, Agroha and Nuh and Pandit Bhagwat Dayal Sharma University of Health Sciences, Rohtak—has shortage of doctors, nurses and paramedic staff.
The DMER had 40.20 percent vacancies for positions of doctors, 23.9 percent for nurses and 62.5 percent for paramedics.
No regular directors and medical superintendents were appointed in any of the medical colleges under the DMER.
ThePrint reached Haryana health minister Arti Rao and additional chief secretary (health) Sudhir Rajpal over the phone and WhatsApp for comment. This report will be updated if and when a response is received.
Anil Vij, who was Haryana’s health and family welfare minister during the audit period, told ThePrint that the CAG report would be studied by the Public Accounts Committee (PAC) of Vidhan Sabha and only then would he be in a position to know the details.
“I have not studied the report so far. Offhand, I can only say that the government sends lists of vacancies to the commission (Haryana Public Service Commission for Group A and Group B posts and Haryana Staff Service Commission for Group C and D) for recruitments and the rest of the recruitment work is done by them. In the past few years, many of the recruitments were held up due to court cases too,” Vij said.
Also Read: Cracking whip on officials with suspensions & salary cuts, Saini govt follows in Khattar’s footsteps
Inconsistent doctor-to-population ratio
Haryana’s healthcare facilities fall short of meeting the IPHS. A gap exists in the number of health facilities such as CHCs, primary health centres (PHCs) and sub-centres (SCs).
Many facilities suffer from delayed construction, poor maintenance and lack of essential medical services and equipment. Infrastructure challenges are exacerbated by deficiencies in planning and coordination, resulting in underutilised or idle healthcare infrastructure.
Haryana’s doctor-to-population ratio is inconsistent with IPHS norms and recruitment delays further strain service delivery. The lack of specialists impacts outpatient department (OPD) services in hospitals, leaving several districts without crucial specialists such as paediatricians, general surgeons and ENT experts. In some health facilities, specialists are completely absent, impacting patient care negatively.
Unused funds, delayed payments
The CAG report said that between 2016 and 2023, Haryana’s health sector faced significant budgetary underutilisation. Funds allocated by both the central and state governments were often left unused, despite healthcare institutions needing additional resources to meet service demands.
Inadequate release and utilisation of funds impacted critical services and delayed payments to vendors, creating barriers in sustaining uninterrupted service delivery. Major programmes such as the Mukhyamantri Muft Ilaaj Yojana (MMIY) reported pending bills due to lack of timely funds, affecting services like CT scans, dialysis and basic laboratory testing.
Emergency, maternity care missing in many health centres
The audit report said that despite the IPHS mandate for essential OPD services, many health centres lack critical services including emergency and maternity care. As a result, healthcare delivery falls short in terms of meeting minimum service standards, impacting the quality of care provided to patients, especially in rural and underserved regions.
“Availability of drugs and medical equipment is sporadic and inconsistent across healthcare facilities. The report notes gaps in inventory management, procurement delays, and the absence of essential medicines in several health centers,” the report read.
It also said that the online drug management information system intended to monitor and manage drug supplies is underutilised.
The state also lacks a central system to monitor and maintain accurate records of available drugs and equipment across institutions, leading to supply inconsistencies.
Lack of inspections, weak waste management protocol
The report said that Haryana’s regulatory mechanisms, such as compliance with the Clinical Establishments (Registration and Regulation) Act, 2010 and biomedical waste management protocols, remain weak. A lack of inspections and an underdeveloped licensing system for healthcare institutions contribute to quality control issues.
The report emphasised the need to adopt the Government of India’s standards for diagnostics and medical laboratories to enhance accountability and service quality in the private sector.
The CAG report further said that Haryana’s healthcare spending as a percentage of its Gross State Domestic Product (GSDP) and overall budget is below the benchmarks set by NHP, 2017. Despite improvements in certain health indicators such as maternal mortality, the state’s progress on SDG-3 targets remains suboptimal.
The audit suggested the need for a more comprehensive approach to healthcare funding and strategic planning to address these disparities and improve public health outcomes.
(Edited by Radifah Kabir)
Also Read: Month after Haryana defeat, shell-shocked Congress yet to appoint CLP leader. What’s behind delay

